
What's Stress Got To Do With It?
Have you ever been told that your FND is a result of stress? I remember when I was told that, and I wasn’t happy with that explanation at all! I AM NOT STRESSED, DANG IT! At that time, I was very out of touch with what my body was feeling, so I probably wasn’t feeling stressed. I had learned to always look calm, cool, and collected, even if underneath it all I wasn’t.
Everyone gets stressed at times. It’s a normal human reaction. Some of us live in chronic states of stress and don’t even notice it. This may be especially true for those of us who grew up in difficult circumstances. We learned to always stay on high alert in order to protect ourselves. This may have translated to hypervigilance in our adult lives.
Living with chronic stress isn’t good for us. It’s been associated with an increased risk for many illnesses, not just Functional Neurological Disorder. Stress causes our bodies to release stress hormones like adrenaline and cortisol, which can lead to inflammation and other harmful effects.
On the flip side, when we can enter a relaxed state, our bodies benefit. Now I know that many of us with chronic illnesses bristle when someone suggests, “Have you tried yoga?”, but there is a reason that many people benefit from practices like yoga, meditation, gratitude, and mindfulness.

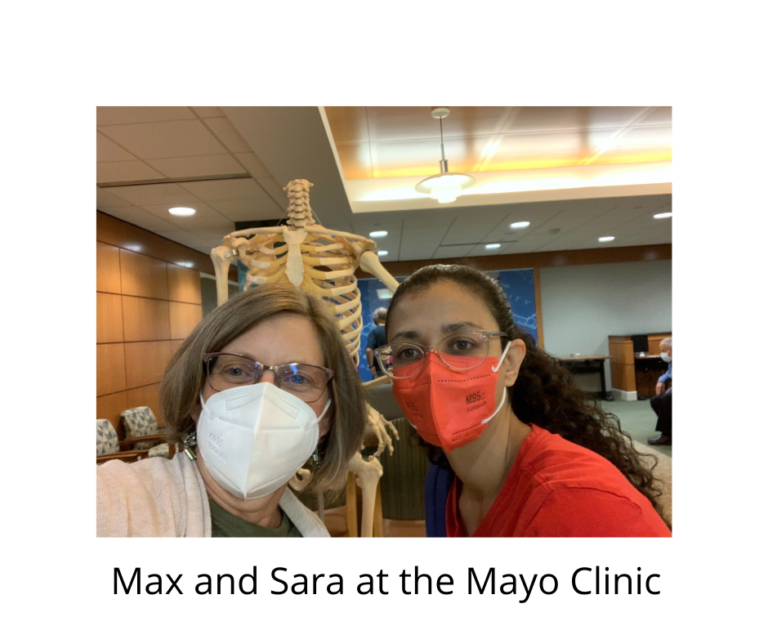
This summer I had the opportunity to go with my friend Sara, blogger at Managing Chronic, to the Mayo Clinic’s BeST program for her FND treatment. We were both a bit surprised that their treatment was focused on using breathing exercises to calm the nervous system. They explained to us that FND symptoms usually occur when our body is in an over-activated state; the sympathetic nervous system is running the show. You’re probably familiar with the term “fight or flight”, which describes how our body sometimes prepares for survival. Other reactions like freezing (my personal reaction of choice) or fawning have been added to the list of survival mechanisms.
When we are in survival mode, our breath is shallow and high in our chest. The therapists at the Mayo Clinic told us that by consciously engaging slow, deep, diaphragmatic breathing, we are helping our nervous system to enter the more relaxed “rest and digest” state regulated by the parasympathetic branch of the nervous system.
This is an especially helpful concept for those of us with Functional Neurological Disorder who struggle with excess body movement. Sara’s primary FND symptom was dystonia, involuntary muscle contractions causing unwanted movements. At first, Sara learned how to perform the abdominal breathing exercises. Once she knew how to calm her breathing, she was told that this was the key to “resetting” her body when symptoms showed up. Whenever she had an involuntary movement, she would stop whatever she was doing and begin her breathing exercise. She continued to practice belly breathing until she could feel that her body was completely relaxed. An important point is to stop and notice what your body feels like in a symptomatic state and compare how it feels to be completely relaxed. As you begin to have greater awareness of this, it becomes easier to spend more time in a relaxed state, and quickly, automatically return to this state when you become aware that you have slipped out of it.
Learning to regulate your nervous system is so beneficial to staying in and increasing your window of tolerance, that zone where your body functions at its best. The more time you stay in this zone, the more you become able to tolerate the ups and downs of life without triggering FND symptoms.
Another reason to stop and “reset” is to prevent reinforcing the abnormal pathways we have developed from Functional Neurological Disorder. Every time we experience an FND symptom, we are strengthening the abnormal pathway. On the other hand, when we perform a movement correctly, we are reinforcing the normal pathway. Thanks to neuroplasticity, we are essentially pruning out the faulty wiring and making it easier to function normally every time that we prevent the abnormal movement and replace it with the correct one. I’ve been taking a mindfulness class recently. My instructor likes to remind us that as we are practicing mindfulness, we are performing brain surgery, no scalpels necessary. Yes, it takes time to engage in practices like mindfulness, meditation, yoga, and breathing exercises, but the results can be life-changing.
While we were at Mayo, we had the privilege of seeing how FND treatment at its best can work. We met someone who had a few weeks before become suddenly unable to walk. Because she lived in the area, she immediately went to Mayo and was diagnosed with FND very quickly. She had the opportunity to be treated by skilled therapists who were very familiar with FND and knew how to help her. She went from wheelchair to walking within a few days with treatment. In my opinion, her prognosis is excellent because she didn’t spend much time in those abnormal pathways. She learned how to handle symptoms if they should show up again, which is the key to living a well-functioning life with FND. This should be the standard of care for FND everywhere!
Sara was a little skeptical that just breathing differently could make a difference in her FND at first, but became a believer in the power of her breath as she saw how her body responded to the practice. Another FND friend of mine recently underwent treatment in London with similar success. “It’s not rocket science, is it?”, she commented to me, meaning that techniques to manage symptoms can seem almost too simple. It seems like such a complex disorder would require complex treatment, but sometimes it’s the simple things that help most. Both of them were surprised and thrilled how well it worked just to learn to attain a relaxed state.
Another way that these techniques work probably is through distraction. When we focus on our symptoms, it’s difficult to control them. Using a breathing practice can help us direct our attention away from symptoms.
If you find it hard to keep focus on your breathing, adding counting to yourself as you breathe (“In, 2,3, Out, 2,3”) or noticing the sensation of the air (feel the coolness breathing in, feel the warmth while breathing out) can help keep attention on the breath. Something we have added to our lives in my mindfulness class is to incorporate a 3 minute breathing routine 3 times a day to our schedule. Since it takes me about 6 seconds for a full inhalation and exhalation, I figured that my slow, deep breathing involves 10 breaths a minute. I thought it would be easy to just count out 30 breaths to complete a 3 minute cycle, but was surprised that I kept getting distracted by about breath 4! Our minds are so busy that it can be tough to stay focused on our breath. It’s become easier with practice.
There are many resources on YouTube or one of the many apps available on your phone. My personal favorites are Calm and Insight Timer, but there are many others. Here’s a breathing meditation I recorded. Give it a try and see how you feel!


19 Comments
As someone with FND And also a peer supporter and mental health advocate at writersdvocatejocelynb.com I wonder if you would give me permission to repost your blog post with links forcing others to access this information to increase the range to include my reach.
Jocelyn Bystrom
Brilliant explanation. We have discovered deep slow diaphragmatic breathing and yinnyoga and meditation to be super helpful. Thank you xox
I’m so glad that you’ve found things that have helped you, Linda! Best wishes for your recovery.
Max
Interesting read, thanks. For me, trying to do diaphragmmatic breathing only serves to focus me on my body’s inability to achieve a more relaxed state. It’s the opposite of distraction and in turn, my spasms intensify. But great if it has a beneficial effect for some.
Thanks for your comment, Lis. Have you noticed times that your body is more relaxed than others? It might be helpful as a first step to just pay attention to the different levels of tension and relaxation that we all experience. Sometimes it takes baby steps to get where we want to be. What do you do that is enjoyable? Where are you when you feel your best? You might want to notice the things that you are saying to yourself and question if there could be statements that would be more beneficial for your recovery. Even though you currently find relaxation difficult, I hope that you find ways to increase that ability.
I’m rooting for you!
Max
Thank you!
Thanks for reading, Lil!
All the best,
Max
This is right spot on…..
Mindfullnes and DBT and a great therapist (THKS BARBARA). I have been reflecting on these skill since 2017.
Good for you, Chuck! I’m glad that you found someone who has helped you on your way!
Wishing you the best of health,
Max
Great that diaphragmmatic breathing helps some people. Personally, I find breathing exercises focus me even more on my body’s struggle to relax, resulting in an increase in muscle spasms. I guess for me, focusing on my breathing is not a beneficial distraction
Sometimes the struggle is real! Maybe you could start a list of activities that are a bit calming for you. My list includes warm baths, time in nature, reading, and snuggling with my dogs. Every time you notice even a little relaxation, pause and pay attention to the feeling. Feel proud of the accomplishment, no matter how small. It isn’t easy, but every small step is a step closer to managing your symptoms.
Wishing you the best,
Max
Good morning
I had an episode at about 00:10 one morning. I was fast asleep and woke up to stroke symptoms. Admitted to hospital for stroke. Diagnosed with FND. My body gave me no warning signs that I was aware of. There is NO expert in South Africa. Any ideas what to look for? Your assistance will be greatly appreciated.
Kind regards
Lilla
Hi Lilla,
That sounds incredibly frustrating! Be sure to check out neurosymptoms.org and FNDHope.org for more great information on FND. I’m sorry you have been left in limbo.
Wishing you the best,
Max
Are there any studies into breathing pattern disorder (+/- sleep apnea) and FND? I suspect there may be a link for some. Not just the ANS system effect, but poss CO2 v O2 driven breathing / blood gasses?
Hi Jean,
I’m not aware of any, but it’s an interesting question.
Max
Hi Max
thank you for this, i did the breathing last night and it actually helped me fall asleep without focusing on my symptoms.
i have had an awful 11 weeks however thankfully i was diagnosed quite early on. I have tingles burning and weird sensations in limbs and sometimes my side. they come and go, move around and for someone who was absolutely fine one day to feeling this the next has been horrendous. I thought i hd MS and got myself in a huge hole with panicking.
this breathing really helped, im doing Yoga, walking, and have massages once a month, baths help and spend time with family and friends as when im distracted symptoms are gone. Im also seeing a counselor who is helping me with my subconscious and tapping skills.
its mice to read about someone’s recovery story and not all doom and gloom you find on google, so thank you so so much
Thank you for your kind comment, Maria. I’m glad that you’re finding things that help you. I think that experiencing panic is common to most of us with FND. It’s normal to be concerned with our symptoms, of course, but once we understand that they are caused by FND, learning to calm our nervous system instead of panicking is crucial to recovery. Best of luck to you as you continue to learn to manage your FND.
Max
How can I find a skilled FND provider in my area?
Hi Wendy,
That can be such a challenge! You can try the provider finder FND Hope offers here- https://fndhope.org/living-fnd/managing-fnd-find-provider/. The FND Society also has a referral search tool. https://www.fndsociety.org/referral/
I hope you find a great provider in your area!
Max